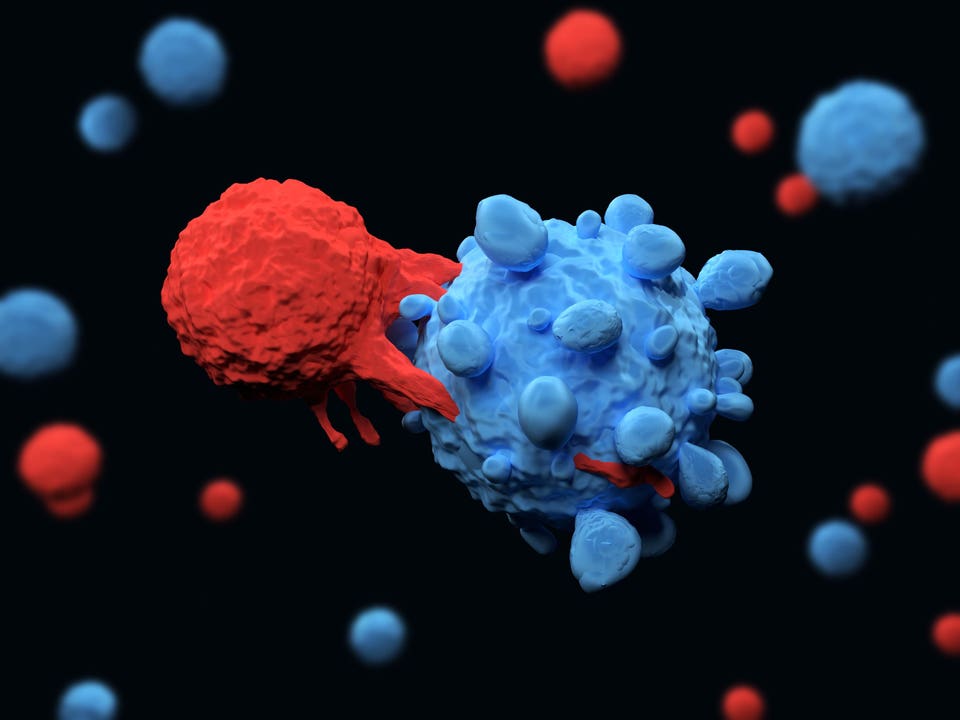
The microbes in our gut can influence our health and may play an important role in determining how patients react to new therapies that engineer their immune system to fight cancer. Immune system T cell attacking a cancer cell. The December 2023 ASH meeting on the impact of the microbiota on immunotherapy and hematological cancers highlighted the link between the gut microbiome and blood cancer treatment.
A panel of scientists from Stanford, UPenn, City of Hope and the Fred Hutchinson Cancer Center discussed the associations among blood cancer treatment by , or CAR T, the use of antibiotics, and the composition of the gut microbiome. While more research is needed, current results suggest that certain antibiotics that disrupt the gut microbiome could modulate treatment and affect patient survival rates. CAR T-cell therapy is designed to trigger the patient’s own immune system against several types of blood cancers, including leukemia and lymphoma.
This is achieved through the genetic modification of immune cells named “ ”, which are responsible for stirring the immune response to execute immune functions. First, T cells are harvested from each patient. Next, these are genetically modified to express “ ” (CARs) that, once reinfused in the patient, can selectively recognize, and destroy cancer cells.
Genetic engineering and gene manipulation. “CAR T cell therapy is a precious tool for the treatment of patients with previously unmet needs, for which first line approaches failed at least twice. Unfortunately, only 30-40% of patients show long term response while others relapse within 5 years.
The treatment itself can also cause systemic inflammation and neurotoxicity. We need to tackle these problems to increase survival rates and improve the quality of life for survivors” explains Marco Ruella MD, senior investigator in a hallmark study and Assistant Professor at the University of Pennsylvania Perelman School of Medicine. It is not well understood why CAR T cell therapy is sometimes ineffective or produces a toxic reaction.
have demonstrated a connection between the gut microbiome and unfavorable outcomes for other types of therapies that leverage the patient’s own immune system against cancer, such as in melanoma, lung, kidney, and bladder cancer. However, these investigations did not clarify whether the association is also valid for CAR T-cell therapy. Intrigued by this hypothesis, Ruella and his collaborators at the Memorial Sloan Kettering Cancer Center started mining archival data from blood cancer patients treated with CAR T cell therapy.
“Our analysis unraveled strong associations between the use of antibiotics and low survival rates,” says Ruella. “Patients that received antibiotics in the four weeks before treatment were relapsing more often and had lower survival rates. We also found that a specific group of was associated with worse survival and increased toxicity.
” To confirm their findings, they performed a prospective study, i. e. , a type of longitudinal investigation where scientists observe a group of patients over a defined period of time to understand how selected factors affect treatment outcomes.
“We collected stool samples from 50 patients receiving treatment and analyzed changes in the composition and diversity of their gut microbiome. Patients with worst outcomes had reduced gut microbiota diversity. We also found that and in the class of the bacteria were associated with better response and reduced toxicity.
” In a , Ruella and coauthors administered vancomycine to B cell acute lymphoblastic leukemia patients, obtaining improved outcomes after CAR T cell therapy across tumor types. Recent peer reviewed work showed that high levels of the same bacteria ( and ) are associated with better patient response to checkpoint inhibitor immunotherapy. This finding extends to translates in patients receiving CAR T cell therapy, with potential important implications for treatment optimization.
However, Ruella cautions that “at this stage we cannot recommend any specific intervention. We need to validate these results in bigger cohorts of patients. This, together with a better understanding of patient’s lifestyle and dietary habits, could lead to the clinical implementation of dietary recommendations for improved efficacy and lower toxicity of CAR T-cell therapy.
” It is evident that a healthy gut microbiome can support therapy and it is possible that the use of some antibiotics could be toxic or enhancing microbiome health. “In the future, we may be able to derive clinical guidelines to prioritize some antibiotics over others, based on their effects on the gut microbiome of cancer patients” he concludes. .
From: forbes
URL: https://www.forbes.com/sites/ameliapalermo/2023/12/18/gut-health-could-play-a-role-in-how-blood-cancer-patients-respond-to-new-therapies/