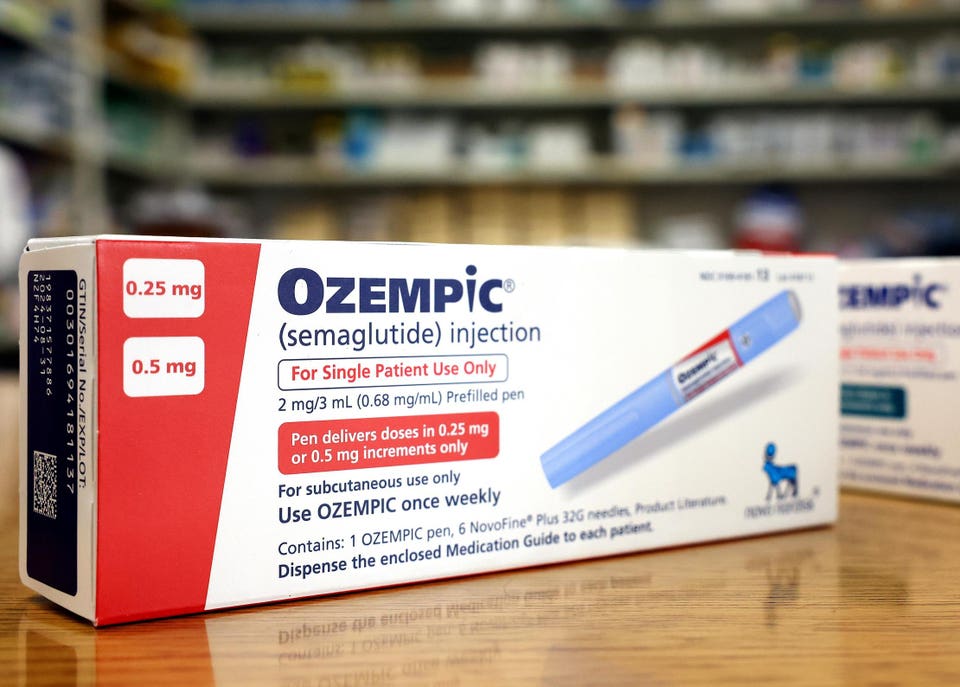
Forbes Innovation Healthcare New Classes Of Obesity Drugs Face Strong Headwinds From Insurers Joshua Cohen Contributor Opinions expressed by Forbes Contributors are their own. I write about prescription drug value, market access, healthcare systems, and ethics of distribution of healthcare resources Following Aug 3, 2023, 07:27pm EDT | Press play to listen to this article! Got it! Share to Facebook Share to Twitter Share to Linkedin LOS ANGELES, CALIFORNIA – APRIL 17: In this photo illustration, boxes of the diabetes drug Ozempic . .
. [+] rest on a pharmacy counter on April 17, 2023 in Los Angeles, California. Ozempic was originally approved by the FDA to treat people with Type 2 diabetes- who risk serious health consequences without medication.
In recent months, there has been a spike in demand for Ozempic, or semaglutide, due to its weight loss benefits, which has led to shortages. Some doctors prescribe Ozempic off-label to treat obesity. (Photo illustration by Mario Tama/Getty Images) Getty Images There’s certainly plenty of demand for and hype around the new wave of weight loss agents.
But health insurers are pulling back on coverage , according to a recent survey published by the obesity care provider Found . Evidently, the results are consistent with national trends in coverage for these products. Insurers are clamping down on coverage.
In payers’ lingo this could mean outright reimbursement denials. It can also imply more subtle ways of limiting their financial exposure. These include the use of step edits to discourage doctors from prescribing the more expensive drugs first; or requiring pre-authorization, usually in the form of a specific diagnosis and data on the patient, such as their body mass index, before dispensing and reimbursing a product.
The new classes of obesity medications—GLP-1 and GIP/GLP-1 receptor agonists—have approved uses for diabetic patients. But they’re being prescribed for obesity both on- and off-label, depending on the drug in question. The drugs include Saxenda (liraglutide), two semaglutide-based agents, Ozempic and Wegovy, and Mounjaro (tirzepatide).
Saxenda and Wegovy have labeled obesity indications, while Ozempic and Mounjaro do not (yet). Found’s research revealed that 69% of its patient population do not have coverage for GLP-1 drugs to treat diabetes or for weight loss. This constituted a 50% decline in coverage since December 2022.
Further, two large U. S. employers recently announced they are no longer placing Wegovy and other weight loss drugs on their formularies.
These employers are Ascension, one of the country’s biggest hospital systems, and the University of Texas. MORE FOR YOU Pfizer Sued By GSK Over Alleged Patent Infringement For Its RSV Vaccine Penicillin Shortage Explained Increased Syphilis Rates And Amoxicillin Shortage Fueled Crisis Pfizer Expects Signoff For New Covid Boosters As Soon As This Month Here s What To Know And Why They re Needed Notably, both employers previously covered weight loss drugs. But they’re backpedaling.
Ascension stopped paying for all weight loss drugs on July 1. The University of Texas intends to ratchet down coverage dramatically, including no longer covering the branded medications Saxenda and Wegovy, by September 1. The University of Texas gave reasons for its decision.
It says that the change in policy is primarily budget-related. Additionally, it states that higher costs would drive up enrollee premiums, which it wants to prevent from happening. Repurposed semaglutide products and tirzepatide have substantially greater efficacy than previous generations of obesity therapeutics.
But there are important questions concerning the products’ side effects and tolerability and potentially serious safety signals , which the European Medicines Agency has posted in recent weeks. These include a possible links to thyroid cancer and suicide ideation. Moreover, in the U.
S. lawsuits were filed this month claiming the drugs caused stomach paralysis or gastroparesis . While the adverse event profile could be a concern to payers, at present the issues that influence their coverage decisions are mostly financial, including the budgetary impact of reimbursing drug costs for large numbers of patients with weight problems and the products’ lack of cost-effectiveness.
In August 2022, the Institute for Clinical and Economic Review, which performs cost-effectiveness assessments in the U. S. , released a report on obesity medicines.
Of the treatments reviewed, the ICER report gave the best ratings to Wegovy and Saxenda. At the same time, ICER did not consider Wegovy cost-effective at the current U. S.
price. At $237,000 per quality-adjusted life-year gained, it is substantially above the $100,000-to-$150,000 range considered the upper bound for cost-effectiveness in the U. S.
And so ICER suggested price cuts to bring Wegovy’s price in line with its value. Specifically, ICER indicated a benchmark annual price range for semaglutide of between $7,500 to $9,800 would make the product cost-effective. Lowering the prices substantially does make the products more cost-effective, as is shown by the positive guidance for Wegovy issued in March of this year by the U.
K. ’s cost-effectiveness watchdog, the National Institute for Health and Care Excellence. This recommendation was based on a much lower price for Wegovy in the U.
K. At £199 ($250) for a month’s supply, Wegovy is appreciably cheaper than the roughly $1,300 it is listed at in the U. S.
Still, NICE’s guidance confines reimbursed usage to a very narrow group of patients, much narrower than the label. In the U. K.
, once supply issues are sorted out, Wegovy will only be available to severely obese adults who have at least one additional weight-related condition, such as heart disease or high blood pressure, a body mass index BMI of more than 35, prescribed only within an National Health Service-authorized specialist weight-management scheme and for a maximum of two years. In the U. S.
insurers have similar cost concerns. Among other things, they’re worried about patients having to take them indefinitely to avoid a rebound effect and the potential for sizeable off-label use. What’s undeniable, however, is that the new drugs, whether repurposed or novel agents such as Mounjaro, have robust clinical effectiveness and can even be cost-effective, depending on the price.
This sets them apart from their predecessors, which weren’t particularly effective and very often had rather unbearable side effects. Obesity is linked with heart disease, stroke, type 2 diabetes and certain types of cancer. Indeed, the indirect impact of weight loss medicines on cardiovascular outcomes is being studied.
The preliminary data suggest positive benefits. If there is more evidence that emerges by next year this could alter the cost-effectiveness profile favorably for the obesity drugs. Nevertheless, in the U.
S. most payers do not have a long-term view. Churn or enrollee turnover, plan members frequently going from one insurer to another, precludes payers from seeing the potential value of these products down the road.
As a result, there’s growing reluctance among commercial insurers to pay for these drugs. And it’s worse in the public markets, which now represent almost half of the entire market. Medicaid hardly pays for any weight loss agents, and Medicare is prohibited from doing so.
Even if Congress were to lift the prohibition on coverage of obesity drugs in Medicare, as may occur in the near future, this would not automatically mean Medicare plans would all pay for them. In fact, most Medicare plans would probably behave like commercial insurers do now. Without insurance coverage, what will patients do? There is no doubt that the drugs can be effective at inducing weight loss.
But they’re expensive, with list prices ranging between $900 and $1,600 a month. And they’re meant to be taken continually. There are limits to what most Americans are able and willing to spend out-of-pocket on such drugs.
Therefore, without coverage it’s a stretch to think that most of those eligible for these drugs will dole out well over $10,000 annually, forever. What’s being observed currently in terms of demand derives mostly from a highly influential group of early adopters. However, this can’t properly foretell what will happen several years from now.
For one thing, most of the people presently being prescribed the obesity drugs are paying for all the costs out-of-pocket. As such, they don’t represent the majority of the populace who will depend on insurance to pay for these drugs. Drug manufacturers may be getting a bit concerned at this point, as not having coverage will considerably limit uptake.
The question then is, could these products become massive blockbusters if insurance carriers open their pocketbooks, if you will? The answer is yes. It could happen. But long-term sales forecasts are invariably subject to a lot of uncertainty.
So when we hear about annual sales projections for obesity drugs of over $100 billion by 2030 we need to pause and reflect on which assumptions underlie the modeled forecasts. Presumably, such modeling presupposes a trend towards more (and not less) coverage of obesity drugs across all markets, commercial and public alike. Follow me on Twitter .
Joshua Cohen Editorial Standards Print Reprints & Permissions.
From: forbes
URL: https://www.forbes.com/sites/joshuacohen/2023/08/03/new-classes-of-obesity-drugs-face-strong-headwinds-from-insurers/