In July, an HIV-positive man became the first volunteer in a clinical trial aimed at using Crispr gene editing to snip the AIDS-causing virus out of his cells. For an hour, he was hooked up to an IV bag that pumped the experimental treatment directly into his bloodstream. The one-time infusion is designed to carry the gene-editing tools to the man’s cells to clear the virus.
Later this month, the volunteer will stop taking the antiretroviral drugs he’s been on to keep the virus at undetectable levels. Then, investigators will wait 12 weeks to see if the virus rebounds. If not, they’ll consider the experiment a success.
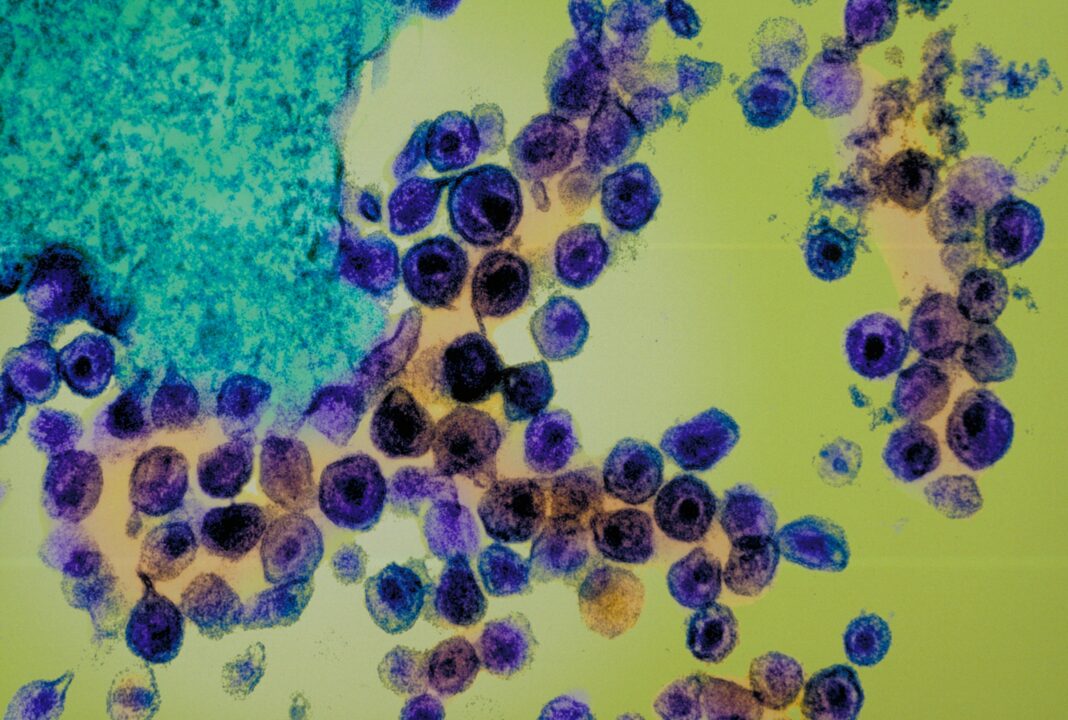
“What we’re trying to do is return the cell to a near-normal state,” says Daniel Dornbusch, CEO of Excision BioTherapeutics, the Philadelphia-based biotech company that’s running the trial. The HIV virus attacks immune cells in the body called CD4 cells and hijacks their machinery to make copies of itself. But some HIV-infected cells can go dormant—sometimes for years—and not actively produce new virus copies.
These so-called reservoirs are a major barrier to curing HIV. “HIV is a tough foe to fight because it’s able to insert itself into our own DNA, and it’s also able to become silent and reactivate at different points in a person’s life,” says Jonathan Li, a physician at Brigham and Women’s Hospital and HIV researcher at Harvard University who’s not involved with the Crispr trial. Figuring out how to target these reservoirs—and doing it without harming vital CD4 cells—has proven challenging, Li says.
While antiretroviral drugs can halt viral replication and clear the virus from the blood, they can’t reach these reservoirs, so people have to take medication every day for the rest of their lives. But Excision BioTherapeutics is hoping that Crispr will remove HIV for good. Crispr is being used in several other studies to treat a handful of conditions that arise from genetic mutations.
In those cases, scientists are using Crispr to edit peoples’ own cells. But for the HIV trial, Excision researchers are turning the gene-editing tool against the virus . The Crispr infusion contains gene-editing molecules that target two regions in the HIV genome important for viral replication.
The virus can only reproduce if it’s fully intact, so Crispr disrupts that process by cutting out chunks of the genome. In 2019, researchers at Temple University and the University of Nebraska found that using Crispr to delete those regions eliminated HIV from the genomes of rats and mice . A year later, the Temple group also showed that the approach safely removed viral DNA from macaques with SIV, the monkey version of HIV.
That was an important step toward testing the treatment in people, says Kamel Khalili, a professor of microbiology at Temple University who led the work and is a cofounder of Excision Biotherapeutics. “You don’t want to eliminate the viral genome but at the same time cause any disruption in another part of the human genome and then create another set of problems for the patients,” he says. “We had to make sure that we identified a region within HIV that did not overlap with the human genome.
” Dornbusch thinks this strategy will spare patients from serious side effects or “off-target” edits—unintentional cuts elsewhere in the genome that could cause problems such as cancer. The regions targeted by the company’s Crispr therapy are also in a part of the genome that tends to stay the same even when HIV evolves. That’s important because the virus mutates rapidly, and the researchers don’t want a moving target.
This isn’t the first time scientists have tried to use gene editing in the hope of curing people with HIV, but other efforts have focused on a protective mutation in a gene called CCR5 . In the 1990s, scientists found that people with this naturally occurring mutation didn’t get HIV when exposed to it. The mutation—known as delta 32—thwarts the virus’s ability to get inside immune cells.
In 2009, California-based Sangamo Therapeutics used an older editing technology called zinc finger nucleases to add that protective mutation into patients’ T cells—an important part of the immune system. Those trials have had limited success . In 2017, Chinese scientists combined Crispr with a bone marrow transplant in an attempt to cure a patient with HIV and leukemia .
In a typical transplant, donor stem cells are transferred to a recipient to replace their cancerous blood cells. These cells go on to form new, healthy blood cells. To also address the patient’s HIV, researchers edited the donor stem cells with Crispr to disable CCR5 .
But after the transplant, only a small percentage of the patient’s bone marrow cells ended up with the desired edit. Then in 2018, Chinese scientist He Jiankui used Crispr to edit the CCR5 mutation into the genomes of twin baby girls to make them resistant to HIV. Fraught with ethical violations , the experiment was widely condemned by scientists .
He’s research was suspended by the Chinese government, and he served a three-year prison sentence. While the twins were born healthy, only some of their cells were successfully edited, meaning the girls might in fact not be immune to HIV. As of 2022, two people have now been cured of HIV after receiving bone marrow transplants from donors with the CCR5 .
Known as the Berlin patient and the London patient , both had cancer and received transplants to treat their disease. But these transplants aren’t a viable option for most people—they’re highly risky, and donors with the delta 32 mutation are scarce. But a third person was declared cured of HIV earlier this year after she received a new type of transplant involving umbilical cord blood.
The Excision trial will eventually enroll nine participants and test three dosage amounts to determine which is most effective. Investigators will measure each person’s viral load and CD4 count before receiving the therapy and after they stop taking antiretroviral drugs. The ultimate goal is to get viral loads down to an undetectable level—that is, less than 200 copies of HIV per milliliter of blood.
At this level, HIV can’t be passed on through sex. The challenge for Excision will be getting Crispr to enough cells to bring HIV down to undetectable levels. The company is using an engineered virus to shuttle the gene-editing components to patients’ HIV-infected CD4 cells.
But so far, there’s little human data on how well Crispr works when it’s delivered directly to the body. “It’s possible that you get the virus to such low levels that if a person’s immune system were intact, they might be able to keep the virus at bay such that they don’t have to take antiretroviral therapy anymore,” says Rowena Johnston, vice president of research for amfAR, the Foundation for AIDS. And even though these drugs are very effective, Johnston says, many people would rather be completely free of the virus.
A single Crispr infusion—if it works—would eliminate the need for daily pills. “People with HIV still live with a lot of stigma and internalized shame,” she says. “I think a cure is something that addresses that much better than lifelong therapy, regardless of how easy that therapy becomes.
”.
From: wired
URL: https://www.wired.com/story/a-bold-effort-to-cure-hiv-using-crispr/