Two months into the international monkeypox epidemic, which so far has caused almost 6,000 infections in the United States and more than 18,000 cases worldwide, it may be old news to say that this disease has visited the US before. In 2003, the virus arrived via exotic pets imported from Ghana, sickening 72 people, including kids as young as 3 years old. It sent 19 people to the hospital before the outbreak burned itself out.
Looking back, the obvious lesson seems to be how much monkeypox has changed its behavior since then. In 2003, every case could be traced back to a person’s exposure to an infected animal. In 2022, transmission appears overwhelmingly person to person , traceable to sexual or skin-to-skin contact among men who have sex with other men.
But there’s a key detail in the 2003 outbreak that worries researchers examining this new one. Two decades ago, the virus spread because it passed from captured African wildlife to American animals being sold for pets. Those pets, wild prairie dogs, transmitted the virus to humans.
No one had considered such cross-species vulnerability because human infections with monkeypox had not previously been detected outside of West and Central Africa. At the time, it was well understood that African wildlife species passed the disease to people who hunted them or lived in their territories. What was surprising was that the virus could be transmitted to the wildlife of other continents.
It remains a cautionary tale—and it may be a warning that the virus could establish itself in new animal populations, now that it has spread to almost 80 countries. This is by no means certain. But it’s enough of a worry that virologists are talking about the possibility of new host species in new territory—spread that might constitute a “spillback” from humans into animals, creating fresh exposure risks beyond what’s currently known.
Scientists are exploring this carefully; no one wants to be inflammatory. “I don’t think there have been any cases at this point that were clearly from zoonotic spillover,” says Angela Rasmussen, a virologist and associate professor at the Vaccine and Infectious Disease Research Organization-International Vaccine Centre at the University of Saskatchewan. “And I do think that that would be distinct, because we would see cases popping up with no connection to an MSM sexual network, and that has not happened yet.
” Because several rodent species have been found to harbor monkeypox in the countries where it was first identified, it’s a reasonable bet that multiple species could be vulnerable to it elsewhere. But there isn’t enough accumulated science to tease out the implications. Could European or American wildlife pick up the disease briefly and then overcome it? Or would it become a persistent infection among them? If it became endemic in wildlife populations, whether that’s prairie dogs in the countryside or rats in cities, could it be transmitted to other species that mix with them? And how close would any of those animals have to come to people to pose an infectious risk—or to be put at risk by human contact? “What I take from the 2003 experience is that there is a diverse range of species that are likely susceptible to monkeypox,” says Jason Kindrachuk, a microbiologist and assistant professor at the University of Manitoba who studies monkeypox and other zoonotic pathogens.
“But we do not yet fully understand what that looks like. ” Though it circulates in a variety of rodent and primate species, monkeypox got its name because the first few times the disease was identified, the victims were monkeys that had been collected for zoos or as research animals. It was first recorded in monkeys shipped from Singapore to a polio-research facility in Copenhagen in 1958 , then in labs at the University of Pennsylvania in 1960 and the US Army’s Walter Reed Institute of Research in 1962 .
Two years later, it sickened an array of monkeys and apes—orangutans, chimpanzees, gorillas, gibbons, and several other species—living in the Rotterdam Zoo . That outbreak conveyed an early warning that monkeypox can move in complex ways because none of the primates arrived at the zoo infected. The virus was passed to them by a new acquisition: two giant South African anteaters sold to the zoo by a wild animal dealer.
It was theorized afterward that, somewhere along their chain of custody, the anteaters were stashed in a holding facility with animals that were already infected—similar to the mixing that would cause the US outbreak in 2003. That might have been the reason the lab monkeys in the first outbreaks were infected too; old medical journals say there was a huge worldwide trade in primates in the 1960s, an unpleasant side effect of the push to manufacture and test the first polio vaccines. “Conditions for shipping and handling were deplorable,” a prominent virologist wrote in the 1990s, “all kinds of animals from different places being crowded together.
” It took a few more years for public health experts to understand that the source of monkeypox was Africa and that the virus could infect humans, and both discoveries were almost accidental. The 1970s marked the start of an intense international campaign to eradicate smallpox in countries where it still lurked. After vaccinators swept through an area, field teams kept watch for any breakthrough cases with smallpox’s distinctive pustules.
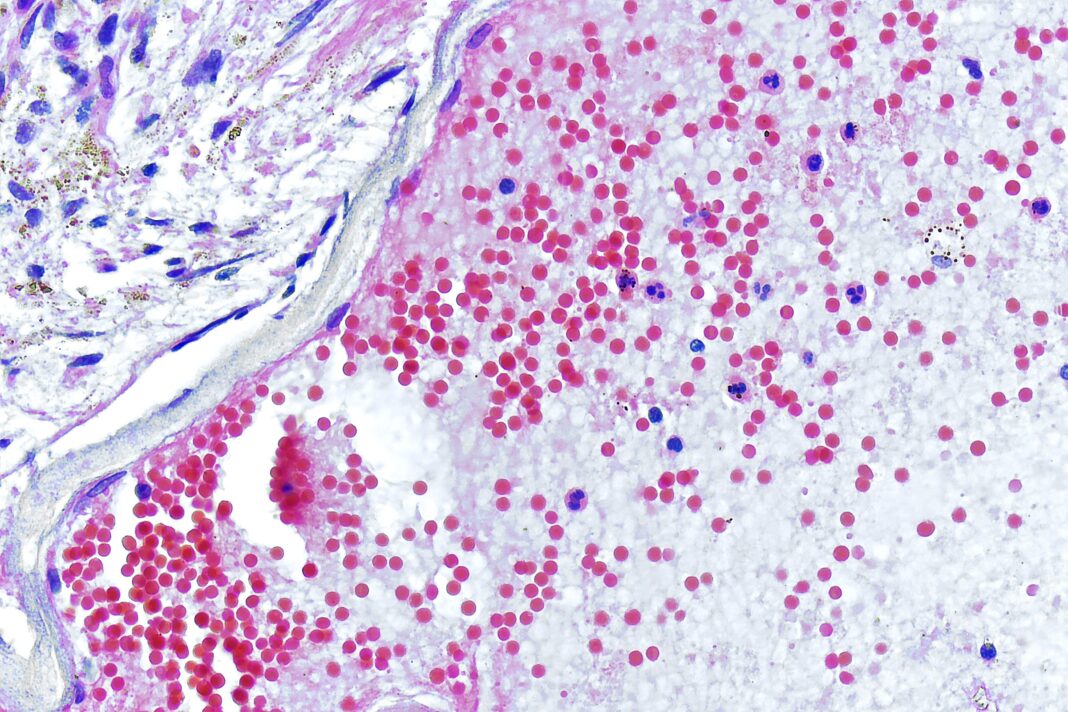
They identified a cluster of cases in a village in the Democratic Republic of the Congo where people were supposed to be fully vaccinated and discovered that the lesions were actually caused by monkeypox. A research project looking for the cluster’s origin started examining local primates—and then realized the virus’s chief harbor might not be monkeys, but rather several species of squirrel that lived on the fringes of villages and were often trapped for food. Decades later, it’s still not clear which rodents or primates are the main hosts of monkeypox, or whether the virus cycles through several species to sustain itself.
There have been only a handful of identifications in animals captured from the wild. Experiments have shown that an array of other species are vulnerable to infection, including mice, guinea pigs, and rabbits. But those lab results can’t address whether these species would become carriers in the real world.
Plus, experimental conditions can be very different from natural ones: Animals may be exposed to a higher viral dose than would happen in the wild, or for a longer period of time. An example of lab conditions that diverge from real-world scenarios is the 2003 situation that caused monkeypox to be released in the US. A succession of exotic-animal dealers housed African species—giant Gambian pouched rats, tree squirrels, and dormice—with American prairie dogs and European hedgehogs, among others.
That contact would have never occurred in a natural ecosystem, and so it may not represent which species would be the most likely hosts if monkeypox took root in the US. (In fact, a 2008 lookback by the US Food and Drug Administration uncovered that more than 170 of the African rodents and 103 prairie dogs linked to the outbreak could not be accounted for afterward. They might have been killed or escaped—but limited sampling in the Midwest did not turn up any further spread.
) The 2003 outbreak isn’t the only time rodents—specifically, pets—have been incriminated in virus transmission. Over the past 20 years, European researchers have repeatedly identified cowpox, a related virus in the orthopox genus, passing to kids from pet rats that may have come from dodgy breeders, or from pet cats who similarly might have been infected at a breeding facility—or might have caught infected rodents and then become infected themselves. There is one documented case of a wild rodent passing that disease to a human, a 14-year-old girl who found an injured rat outdoors and tried to nurse it back to health.
(The rat died. The girl survived. ) Cowpox is more widely distributed than monkeypox and shows up in different parts of the world—Europe and Russia, rather than Africa.
So those occurrences don’t prove the case that monkeypox will follow the same path its viral relative did. But researchers consider those cowpox cases illustrative of the ways infections can cross from the wild world into the human one: in a virus’s home range through close exposure and hunting or far from its original territory, thanks to accidental importation and the exotic-animal trade. “Kids in Germany and France wanted pet rodents, just like the kids in the US in 2003, and that began a trade of potentially infected animals into Germany and France,” says James Diaz, a physician and professor at Louisiana State University’s School of Public Health who has written scientific assessments of rodents as transporters of disease.
Sometimes the door swings both ways. There is good evidence that SARS-CoV-2, the viral cause of Covid, has spilled back from infected humans into animals in North America and Europe—minks and also white-tailed deer, species the virus did not inhabit in its original home in China. It is possible monkeypox could take a similar path.
Early in this epidemic, the UK’s Health Security Agency recommended that people infected with monkeypox remove any pet rodents from their homes until they recover to reduce the chance of spillback. In the US, the Centers for Disease Control and Prevention expanded on that, recommending that “people with monkeypox avoid interacting with animals and find someone else to take care of their pets while they recover. ” There’s so little pre-existing data on various species’ vulnerability to monkeypox that the only way to define the risks may be to set up broad surveillance programs to find animals with evidence of current or past infections.
That would be a mammoth undertaking, even if scientists knew which species are at risk. “Think about bats and Ebola: We’ve been looking for infections for decades now,” Kindrachuk says. “You’re looking for a tiny, tiny pin in a massive haystack.
” Unlike humans—or mice, for that matter—there are no huge, pre-existing banks of cells and tissues taken over decades from many wildlife species. If those existed, they could provide fodder for comparisons between the known hosts of monkeypox and other species that might be vulnerable. New animal surveillance programs would be difficult to set up and expensive to implement; think of the cost and labor involved in climbing into caves to swab bats for coronaviruses or netting birds to take blood samples that might reveal West Nile.
To detect the spread of monkeypox to new animal species, virologists may have to devise an equivalent of the wastewater sampling set up to detect SARS-CoV-2. Something, in other words, that can use an existing system—in this case, veterinary field research or animal rehab work or zoos—to ask questions that can be answered with rapid, automated lab techniques. That might be less precise than trapping individual animals and swabbing or bleeding them, but it would be faster.
And it would be much faster than the 2003 alternative: not knowing which animals are vulnerable to infection and discovering too late that they are sick. .
From: wired
URL: https://www.wired.com/story/monkeypox-originated-in-animals-could-it-spill-back-into-them/