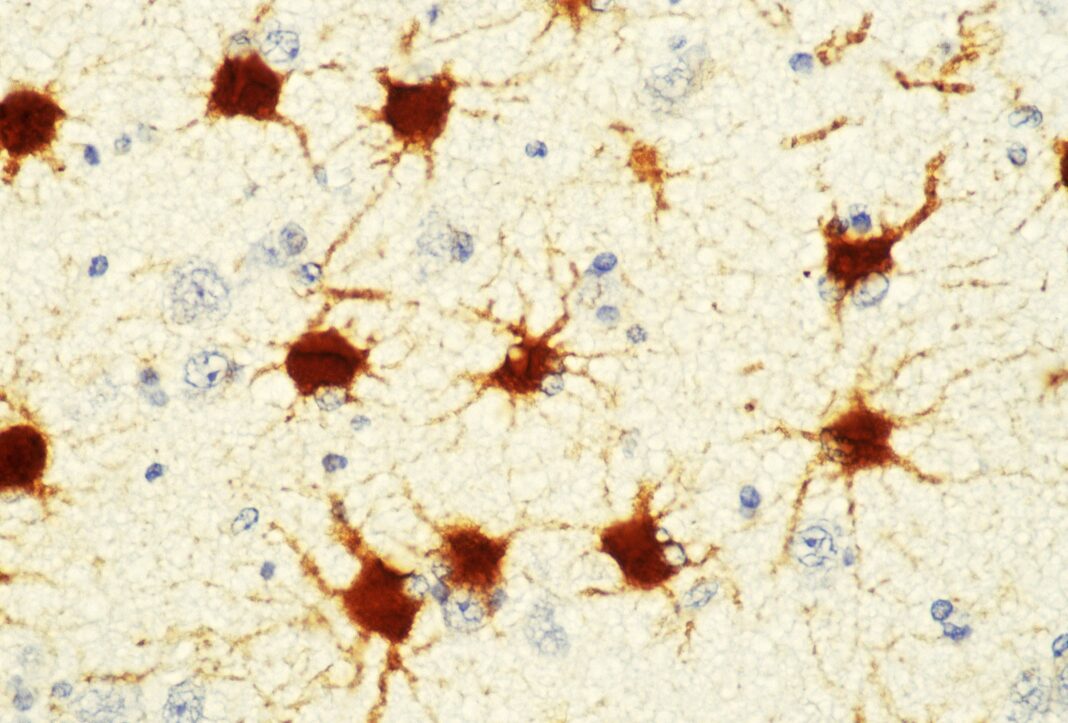
Imagine the brain as the night sky—an expansive sea of tissue dotted with cells of all shapes and sizes. Perhaps the most well known are the filamentous neurons that intertwine with their neighbors to transmit electrical information. A lesser-known type is the astrocyte, a somewhat star-shaped cell that secretes proteins critical for proper brain development.
Astrocytes “tell the neurons what to do,” says Nicola Allen, a neuroscientist at the Salk Institute for Biological Studies. “That’s the big reason we’re interested in them. ” These starry astrocytes are known to play a role in neurodevelopmental disorders such as Down syndrome and Fragile X syndrome.
But exactly how they contribute is an open question—one that Allen’s group has tried to answer by analyzing astrocytes from the brain cells of mice with various disorders. Through a combination of RNA sequencing and proteomics (the large-scale analysis of proteins), they have discovered that these astrocytes secrete larger-than-expected quantities of proteins that are key to neural development. Recently published in Nature Neuroscience , their work identifies several proteins that the scientists think may lead to therapeutic avenues in the future.
“It’s easy to think that neurons are the only cells that matter,” says Alison Caldwell, a coauthor on the study and a former graduate student in Allen’s lab. “But half of the cells in the brain are not neurons—they’re all these other kinds of cells. ” Previous research had shown that trying to grow only neurons in a dish truncated their development.
But if astrocytes—or the proteins released by them—were added, the neurons would be able to undergo more of what’s called neurite outgrowth: They would extend spindly tendrils to form the network necessary for neural communication. Katie Baldwin, a neuroscientist at the University of North Carolina at Chapel Hill, says astrocytes are “master multitasker cells,” and that they “orchestrate neural circuit formation by providing cues in the right place and at the right time. ” In brains with neurodevelopmental disorders, however, these astrocytes may be dysfunctional.
By figuring out what exactly is wrong with the astrocytes, Allen and Caldwell hoped to better understand what is happening in the larger system of the brain. First, the scientists isolated astrocytes taken from mice who had one of three neurodevelopmental disorders: Rett’s syndrome, Down syndrome, and Fragile X syndrome. (In humans, symptoms of Fragile X include speech delays, learning disabilities, and issues with muscle coordination, while Rett’s syndrome can manifest with loss of speech, slowed rate of growth, and breathing issues.
Down syndrome symptoms can include delayed speech and development. ) The lab members had noticed that neurons of animals with any of the three conditions showed less neurite outgrowth and less synapse formation—a hint that dysregulated astrocytes could be involved. To pick out the astrocytes, the team used a procedure called immunopanning—antibodies were used to stick to certain cell types, filtering them out, round by round, until the astrocytes were the only cells left.
Then, the scientists cultured them in petri dishes for a few days. This allowed the astrocytes to start oozing proteins into the media, or the liquid they were being cultured in. The scientists collected the ooze and analyzed it with a mass spectrometer to determine which proteins were in it.
They also ran RNA sequencing on some of these astrocytes to determine their gene expression, comparing it against that of normal cells. This was slow going. “We spent a lot of time, probably the first couple of years, really just working out the immunopanning and culturing the astrocytes,” recalls Caldwell.
One challenge was making sure that the media contained few proteins to start with—those would have interfered with their measurements. The scientists also needed to make sure that culturing the astrocytes in a petri dish would not change their behavior from how they would have acted in the brain. Once they’d established that the cultured cells behaved normally and maintained their ability to direct neuronal development, the scientists looked at the proteins they made and the genes they expressed.
Then they compared those to normal cells. Across all three disorder models, they found 88 proteins, and approximately 11 genes, that were upregulated—meaning their quantity or expression increased. Both Caldwell and Allen were surprised that the two were often out of sync.
While one might think that an increase in a gene’s expression would correlate with an increase in the protein associated with it, this wasn’t exactly the case. Across the three disorders, there wasn’t much overlap between the genes that were most overexpressed and the proteins that were most overproduced. “I think it really highlights, particularly for different disorders, that you’ve really got to look at protein,” Allen says, rather than focusing on gene expression alone.
Baldwin, who was not involved in the study, concurs—noting that this lack of overlap is a “striking” result. “What sequencing can’t capture, that proteomics can, is all the regulation that occurs when the protein is produced,” she says. Sequencing tells you which gene transcripts are available, she adds, but “doesn’t necessarily tell you which ones are being turned into protein, or at what rate they are being turned into protein.
” Allen’s team focused on a few particular proteins that had spiked across all three disorder models. One is called Igfbp2, which inhibits the gene pathway for insulin-like growth factor (IGF)—a hormone that normally aids in brain development. “The idea was that there was too much of this inhibitor being made by the astrocytes,” says Allen.
So the lab tried suppressing it. They gave living mice with Rett’s syndrome an antibody that blocked Igfbp2, and they found that their neurons grew more normally. Another protein that was overproduced in all three animal models is called Bmp6.
It’s thought to regulate astrocyte maturation. Again, the team tested what happened when they turned the protein down. First, they placed mouse neurons in a dish, then added the proteins secreted by astrocytes from mice with Fragile X.
The neurons weren’t able to grow many neurite tendrils. But when the scientists tried again, this time with the ooze from Fragile X astrocytes treated with a Bmp6 inhibitor, those tendrils grew. Knocking out production of the Bmp6 protein seemed to lead to more normal neuron development.
And as it turns out, the two proteins may be interconnected—turning up Bmp6 may also turn up Igfbp2, Allen says, “and that is leading to some of these deficits. ” Baldwin notes that focusing on both proteins and gene expression is “really powerful,” allowing Allen’s team to identify critical factors, like the role of these two proteins, that otherwise might have been missed. “This study really shows why it’s important to consider a lot of different angles when you’re asking these kinds of questions,” agrees Caldwell.
Nathan Smith, a neuroscientist at the University of Rochester who was unaffiliated with the study, says that this work is “helping to push the field forward” by showing that disrupting the crosstalk between neurons and astrocytes can lead to neurological disorders. “This gives opportunities to strategically target astrocytes,” he adds, rather than “just focusing on neurons. ” For Caldwell and Allen, these results have opened many new directions for future research.
One is to explore whether Igfbp2 inhibitors could be delivered to the brain as a treatment for Rett’s syndrome. The Igfbp2 blocking antibody used in the mouse experiments is very large, so the scientists are interested in finding something smaller that more easily crosses the highly protective border between the bloodstream and the brain. Another direction, Allen notes, is to cycle through the proteins identified in this study and look at their specific roles in other disorders.
Igfbp2, for example, “shows up in a lot of different brain disorders, including ones you’d typically associate with aging and regeneration—like Alzheimer’s disease,” she says. “So we’re interested in understanding more about the mechanism of how it’s working, and what it’s doing in these different disorders. ” Caldwell hopes that the other proteins identified in their experiments might also help map out the complexity of an astrocyte’s role in disorders—or even during normal brain development.
“I’m really hopeful that people will find it to be a valuable resource,” she says. “They can start to look at some of these other proteins and try to figure out what their roles are in the brain, and why astrocytes make them. ”.
From: wired
URL: https://www.wired.com/story/to-understand-brain-disorders-consider-the-astrocyte/